Explore effective homeopathic remedies for endocarditis to enhance heart health in this detailed guide.
Introduction
Endocarditis is a serious and potentially life-threatening condition characterized by the inflammation of the inner lining of the heart chambers and heart valves, known as the endocardium. This inflammation is typically caused by an infection, but it can also result from non-infectious processes. Understanding the symptoms, causes, effects, prevention, and homeopathic remedies for endocarditis is crucial for managing the condition and improving outcomes. This article provides an in-depth look at endocarditis, offering insights into its complexities and the role of homeopathy in its treatment.
1. Understanding Endocarditis
1.1 What is Endocarditis?
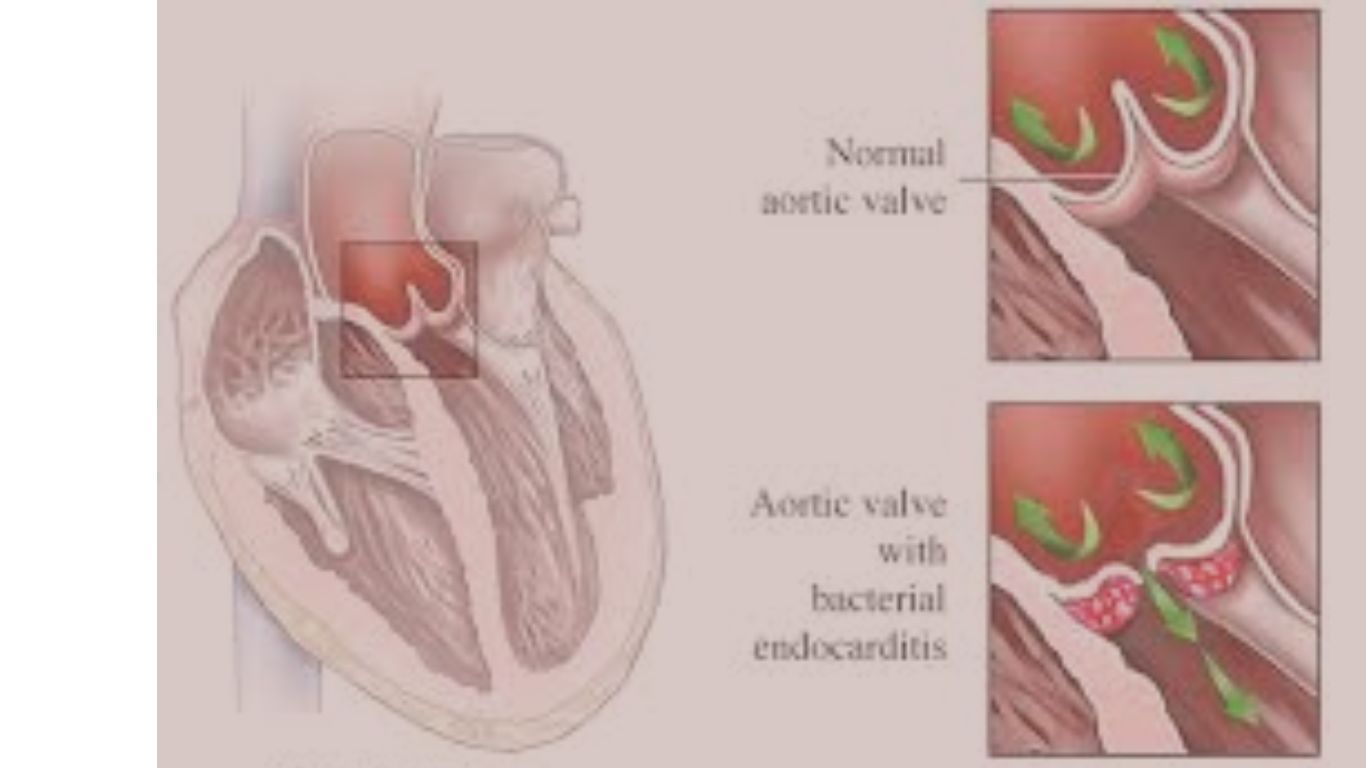
Endocarditis is an inflammation of the endocardium, the inner lining of the heart chambers and valves. The condition is most commonly caused by an infection, which can lead to the formation of clumps of bacteria, immune cells, and blood clots on the heart valves. These clumps, known as vegetations, can interfere with the normal functioning of the heart valves and can be life-threatening if not treated promptly.
There are two main types of endocarditis:
- Infective Endocarditis (IE): This is the most common form of endocarditis and is usually caused by bacterial infections. It can also be caused by fungi and other microorganisms.
- Non-Infective Endocarditis: This type is less common and may be associated with autoimmune diseases, cancer, or other non-infectious conditions.
2. Symptoms of Endocarditis
The symptoms of endocarditis can vary widely depending on the type of endocarditis, the causative organism, and the individual’s underlying health condition. Symptoms can be subtle and develop slowly over time (subacute endocarditis) or appear suddenly and progress rapidly (acute endocarditis).
2.1 Common Symptoms
- Fever and Chills: Persistent or intermittent fever is the most common symptom of infective endocarditis. It is often accompanied by chills and night sweats.
- Fatigue: Severe fatigue and weakness are common, often making it difficult for the individual to perform daily activities.
- Heart Murmurs: A heart murmur, an abnormal sound heard during a heartbeat, may be a sign of endocarditis, particularly if it is new or has changed from a previous murmur.
- Shortness of Breath: Difficulty breathing, especially during physical activity, may occur due to heart valve damage and heart failure.
- Chest Pain: Some individuals may experience chest pain, particularly if the infection affects the heart’s outer lining (pericardium).
- Cough: A persistent cough may develop, sometimes accompanied by blood-streaked sputum.
- Swelling: Swelling of the legs, abdomen, or other areas of the body can occur due to heart failure.
- Weight Loss: Unintentional weight loss is a common symptom of subacute endocarditis.
2.2 Other Symptoms
- Petechiae: Small, red or purple spots on the skin, mucous membranes, or the whites of the eyes may appear due to tiny blood clots.
- Osler’s Nodes: Painful, red nodules may develop on the pads of the fingers and toes.
- Janeway Lesions: Painless, flat, red spots may appear on the palms of the hands or soles of the feet.
- Splinter Hemorrhages: Small, dark streaks may be visible under the fingernails or toenails.
- Roth Spots: Retinal hemorrhages with pale centers, known as Roth spots, may be observed during an eye examination.
3. Causes of Endocarditis
Endocarditis is primarily caused by an infection, but it can also result from non-infectious processes. The causes can be broadly categorized into infectious and non-infectious.
3.1 Infectious Causes
- Bacterial Infections: Bacterial endocarditis is the most common form of the condition. The bacteria that most often cause infective endocarditis include:
- Streptococcus viridans: Commonly found in the mouth, these bacteria can enter the bloodstream during dental procedures or with poor oral hygiene.
- Staphylococcus aureus: Often found on the skin, this bacterium can enter the bloodstream through cuts, wounds, or intravenous drug use.
- Enterococci: These bacteria are normally found in the gastrointestinal tract and can cause endocarditis in individuals with underlying gastrointestinal or genitourinary infections.
- HACEK group bacteria: These are a group of fastidious Gram-negative bacteria that can cause endocarditis, particularly in individuals with pre-existing heart conditions.
- Fungal Infections: Fungal endocarditis is less common but can occur in individuals with weakened immune systems, those who have undergone heart surgery, or those with intravenous drug use. The most common fungi involved are Candida and Aspergillus species.
- Viral Infections: While rare, certain viral infections can lead to endocarditis, particularly in individuals with compromised immune systems.
3.2 Non-Infectious Causes
- Autoimmune Diseases: Conditions such as systemic lupus erythematosus (SLE) can cause non-infective endocarditis, known as Libman-Sacks endocarditis. This is characterized by sterile vegetations on the heart valves.
- Malignancy: Some cancers, particularly those affecting the blood or immune system, can lead to non-infective endocarditis.
- Hypercoagulable States: Conditions that increase the risk of blood clot formation, such as antiphospholipid syndrome, can cause non-infective endocarditis.
4. Effects of Endocarditis
Endocarditis can have severe and potentially life-threatening effects on the heart and other parts of the body. The severity of these effects depends on the type of endocarditis, the causative organism, the timeliness of treatment, and the individual’s overall health.
4.1 Cardiac Effects
- Heart Valve Damage: One of the most significant effects of endocarditis is damage to the heart valves. The infection can cause the valves to become perforated, leading to valvular insufficiency (regurgitation) or stenosis (narrowing). This can result in heart failure, as the heart struggles to maintain adequate blood flow.
- Heart Failure: Endocarditis can lead to heart failure if the infection severely damages the heart valves or heart muscle. Heart failure occurs when the heart is unable to pump enough blood to meet the body’s needs, leading to symptoms such as shortness of breath, fatigue, and swelling.
- Myocardial Abscess: The infection can spread to the heart muscle, leading to the formation of abscesses. These abscesses can further damage the heart and may require surgical intervention.
- Conduction Abnormalities: If the infection affects the conduction system of the heart, it can lead to arrhythmias (irregular heartbeats) or heart block, a condition where the electrical signals that control the heartbeat are delayed or blocked.
4.2 Systemic Effects
- Embolism: Pieces of the infected vegetations can break off and travel through the bloodstream, leading to embolism. An embolism can block blood flow to vital organs, such as the brain, lungs, kidneys, or spleen, leading to serious complications like stroke, pulmonary embolism, kidney damage, or splenic infarction.
- Sepsis: Endocarditis can lead to sepsis, a life-threatening condition characterized by a widespread infection that triggers a severe immune response. Sepsis can cause multiple organ failure and requires immediate medical intervention.
- Immune Complex Deposition: In some cases, immune complexes (antigen-antibody complexes) formed during the infection can deposit in the blood vessels, kidneys, and other organs, leading to conditions such as glomerulonephritis (kidney inflammation) or vasculitis (blood vessel inflammation).
- Splenomegaly: The spleen may become enlarged due to the immune response to the infection. In some cases, an abscess may form within the spleen, which can cause pain and may require surgical drainage.
4.3 Long-Term Effects
- Chronic Heart Disease: Even with successful treatment, some individuals may be left with chronic heart disease, such as heart valve damage or heart failure, which may require long-term management or surgical intervention.
- Recurrent Infections: Individuals who have had endocarditis are at increased risk of developing the condition again, particularly if they have underlying heart conditions or do not receive appropriate prophylaxis before invasive procedures.
- Psychosocial Impact: The long-term effects of endocarditis can have a significant impact on an individual’s quality of life, leading to emotional and psychological challenges, such as anxiety, depression, and fear of recurrence.
5. Prevention of Endocarditis
Preventing endocarditis involves addressing the risk factors, practicing good hygiene, and taking precautions during medical or dental procedures, especially for individuals at high risk.
5.1 Good Oral Hygiene
- Regular Dental Care: Maintaining good oral hygiene is crucial for preventing bacterial endocarditis, particularly for individuals with heart conditions. Regular dental check-ups and cleanings can help prevent the buildup of bacteria in the mouth that can enter the bloodstream and cause infection.
- Proper Oral Hygiene Practices: Brushing teeth at least twice a day, flossing daily, and using an antiseptic mouthwash can reduce the risk of oral infections that could lead to endocarditis.
5.2 Prophylactic Antibiotics
- Antibiotic Prophylaxis: Individuals with certain heart conditions or who have had endocarditis in the past may be prescribed prophylactic antibiotics before undergoing dental procedures or other invasive procedures that could introduce bacteria into the bloodstream. Conditions that may warrant antibiotic prophylaxis include:
- Prosthetic heart valves or valve repair with prosthetic material
- Previous history of infective endocarditis
- Congenital heart disease with cyanosis or with prosthetic material
- Heart transplant recipients who develop heart valve disease
- Consulting Healthcare Providers: It is important for individuals with heart conditions to consult their healthcare provider before undergoing any medical or dental procedures to determine if prophylactic antibiotics are necessary.
5.3 Management of Underlying Conditions
- Heart Condition Management: Proper management of underlying heart conditions, such as congenital heart disease, valvular heart disease, or heart failure, can reduce the risk of developing endocarditis. Regular monitoring, medication adherence, and lifestyle modifications are essential components of managing heart health.
- Intravenous Drug Use: Intravenous drug use is a significant risk factor for endocarditis. Individuals who use intravenous drugs should seek support for addiction treatment and practice harm reduction strategies, such as using clean needles and avoiding shared equipment.
5.4 Avoiding Infections
- Prompt Treatment of Infections: Prompt treatment of infections, such as skin infections, respiratory infections, or urinary tract infections, can prevent the spread of bacteria to the bloodstream and reduce the risk of endocarditis.
- Vaccinations: Staying up to date with vaccinations, particularly for conditions such as influenza, pneumonia, and hepatitis, can reduce the risk of infections that could lead to endocarditis.
6. Homeopathic Remedies for Endocarditis
Homeopathy is a holistic approach to medicine that aims to stimulate the body’s natural healing processes. Homeopathic remedies are selected based on the individual’s symptoms, constitution, and overall health. While homeopathy can be used as a complementary approach to conventional medicine, it is important to note that it should not replace medical treatment for endocarditis, especially in acute or severe cases.
6.1 Commonly Used Homeopathic Remedies
- Arsenicum Album: This remedy is often used for individuals who experience great weakness, restlessness, and anxiety, particularly when symptoms worsen at night. It may be indicated for cases of endocarditis where there is a sense of suffocation, palpitations, and a weak pulse.
- Digitalis Purpurea: Digitalis is used for heart conditions characterized by a weak, irregular, or slow pulse. It may be indicated in cases of endocarditis with symptoms of heart failure, such as shortness of breath, palpitations, and edema.
- Cactus Grandiflorus: This remedy is indicated for heart conditions where there is a sensation of constriction or tightness in the chest, as if the heart is being compressed by an iron band. It may be helpful in cases of endocarditis with associated angina or palpitations.
- Lachesis Mutus: Lachesis is used for circulatory and cardiac conditions, particularly where there is a tendency toward clot formation. It may be indicated in cases of endocarditis where there is a sense of constriction, tightness, or oppression in the chest, along with difficulty breathing.
- Spigelia Anthelmia: This remedy is indicated for sharp, stabbing chest pain that radiates to the left arm or shoulder, resembling the symptoms of endocarditis. It may be used for heart conditions associated with pericarditis or valvular heart disease.
- Naja Tripudians: Naja is used for heart conditions with valvular insufficiency or a history of rheumatic heart disease. It may be indicated in cases of endocarditis with symptoms of palpitations, chest pain, and a sensation of suffocation.
- Kalmia Latifolia: This remedy is indicated for heart conditions with shooting pain in the chest, particularly when the pain extends to the left arm. It may be helpful in cases of endocarditis with associated rheumatic fever.
6.2 Homeopathic Case-Taking and Individualization
Homeopathy is highly individualized, meaning that the selection of a remedy is based on the unique symptoms and constitution of the individual. A homeopath will take a detailed case history, including physical, emotional, and mental symptoms, before prescribing a remedy. The goal is to find the remedy that best matches the individual’s overall symptom picture, rather than treating the disease itself.
6.3 Complementary Role of Homeopathy
While homeopathy may offer supportive care during the recovery phase of endocarditis, it is crucial to understand that it should not be used as a substitute for medical care, particularly in acute or life-threatening situations. Endocarditis requires prompt medical treatment, including antibiotics, and in some cases, surgery. Homeopathy can be used alongside conventional treatment to help strengthen the body’s natural defenses, support recovery, and alleviate symptoms, but it should always be done under the guidance of a qualified healthcare provider.
FAQs about Homeopathic Remedies for Endocarditis
Q1: What is endocarditis, and can homeopathy help in its treatment?
A1: Endocarditis is an infection or inflammation of the inner lining of the heart chambers and valves, often caused by bacteria entering the bloodstream. Homeopathic remedies aim to support the body’s natural immune response and reduce inflammation. However, endocarditis is a serious condition that requires immediate conventional medical treatment, such as antibiotics or surgery. Homeopathy can be used as a complementary therapy to aid recovery but should not replace conventional treatment.
Q2: Which homeopathic remedies are commonly recommended for endocarditis?
A2: Common homeopathic remedies for conditions related to endocarditis include Arsenicum Album for weakness and fatigue, Cactus Grandiflorus for chest pain and heart-related symptoms, Lachesis Mutus for circulatory issues and clotting tendencies, and Spigelia for sharp chest pains. The selection of remedies depends on the individual’s specific symptoms and overall health condition.
Q3: Are homeopathic remedies safe to use for endocarditis?
A3: Homeopathic remedies are generally considered safe due to their high dilution, making significant side effects rare. However, due to the serious nature of endocarditis, these remedies should only be used under the supervision of a qualified homeopath and in conjunction with conventional medical treatments to ensure safety and efficacy.
Q4: Can homeopathy prevent endocarditis from recurring?
A4: Homeopathy may help strengthen the immune system and address underlying factors that could contribute to the recurrence of infections, including endocarditis. Remedies like Echinacea are often used to boost immunity. However, preventing endocarditis primarily involves maintaining good dental hygiene, managing underlying heart conditions, and following your doctor’s advice on antibiotic prophylaxis when necessary.
Q5: How does homeopathy complement conventional treatments for endocarditis?
A5: Homeopathy can complement conventional treatments for endocarditis by helping to manage symptoms, support the immune system, and promote overall well-being. For example, remedies might be used to reduce fatigue, anxiety, or chest discomfort that persists after the initial infection has been treated. It’s important that any homeopathic treatment is coordinated with your healthcare provider to avoid potential interactions or complications.
Q6: Can homeopathy be used as a standalone treatment for endocarditis?
A6: No, homeopathy should not be used as a standalone treatment for endocarditis. This condition is life-threatening and requires immediate medical intervention, such as antibiotics or surgery. Homeopathy may be used as an adjunct therapy to support recovery and alleviate certain symptoms, but conventional medical treatment is essential.
Q7: How long does it take to see improvements with homeopathic treatment for endocarditis?
A7: The response to homeopathic treatment can vary based on the individual’s overall health, the severity of the condition, and the specific remedies used. Some patients may notice improvements in symptoms like fatigue or chest discomfort within a few weeks, while others may require longer treatment. It is crucial to continue with conventional medical treatment and regular monitoring by a healthcare professional during this time.
Q8: What precautions should be taken when using homeopathic remedies for endocarditis?
A8: When using homeopathic remedies for endocarditis, it is vital to continue all prescribed conventional treatments and follow your doctor’s advice closely. Homeopathic remedies should be chosen and prescribed by a qualified homeopath, considering the specific symptoms and overall health condition. Patients should never delay or forgo conventional medical treatment in favor of homeopathy when dealing with endocarditis.
Q9: Can homeopathy help with the after-effects of endocarditis, such as fatigue or weakness?
A9: Yes, homeopathy may help address the after-effects of endocarditis, such as lingering fatigue, weakness, or chest discomfort. Remedies like Arsenicum Album and China Officinalis are often used to support recovery from severe infections and restore energy levels. These remedies should be part of a comprehensive recovery plan under the guidance of a healthcare provider.
Q10: What lifestyle changes should accompany homeopathic treatment for endocarditis?
A10: In addition to homeopathic treatment, patients recovering from endocarditis should adopt lifestyle changes that support heart health and reduce the risk of further infections. This includes maintaining good dental hygiene, eating a heart-healthy diet, avoiding tobacco use, managing stress, and following a regular exercise routine as advised by a healthcare provider. Regular follow-up care is also essential to monitor heart health and prevent recurrence.
7. Conclusion
Endocarditis is a serious condition that requires prompt recognition, treatment, and prevention. Understanding the symptoms, causes, and effects of endocarditis can help individuals take proactive steps to reduce their risk and improve their heart health. Preventive measures, such as maintaining good oral hygiene, managing underlying heart conditions, and seeking appropriate medical care before invasive procedures, are essential for reducing the risk of endocarditis.
While homeopathy can play a complementary role in the management of endocarditis, it is important to recognize the limitations of this approach and to prioritize conventional medical treatment in acute or severe cases. By combining preventive strategies, medical care, and supportive homeopathic remedies, individuals can protect their heart health and reduce the likelihood of developing endocarditis, ultimately leading to a longer, healthier life.