Coronary Thrombosis and Myocardial Infarction: A Comprehensive Guide
Introduction
Coronary thrombosis, often synonymous with myocardial infarction (MI) or more commonly known as a heart attack, is a life-threatening condition that results from the sudden blockage of a coronary artery. This blockage prevents oxygen-rich blood from reaching the heart muscle, leading to damage or death of the tissue. Myocardial infarction is one of the leading causes of death globally, and understanding its symptoms, causes, effects, prevention, and treatment, including homeopathic remedies, is crucial for managing and reducing its incidence.
1. Understanding Coronary Thrombosis and Myocardial Infarction
1.1 What is Coronary Thrombosis?
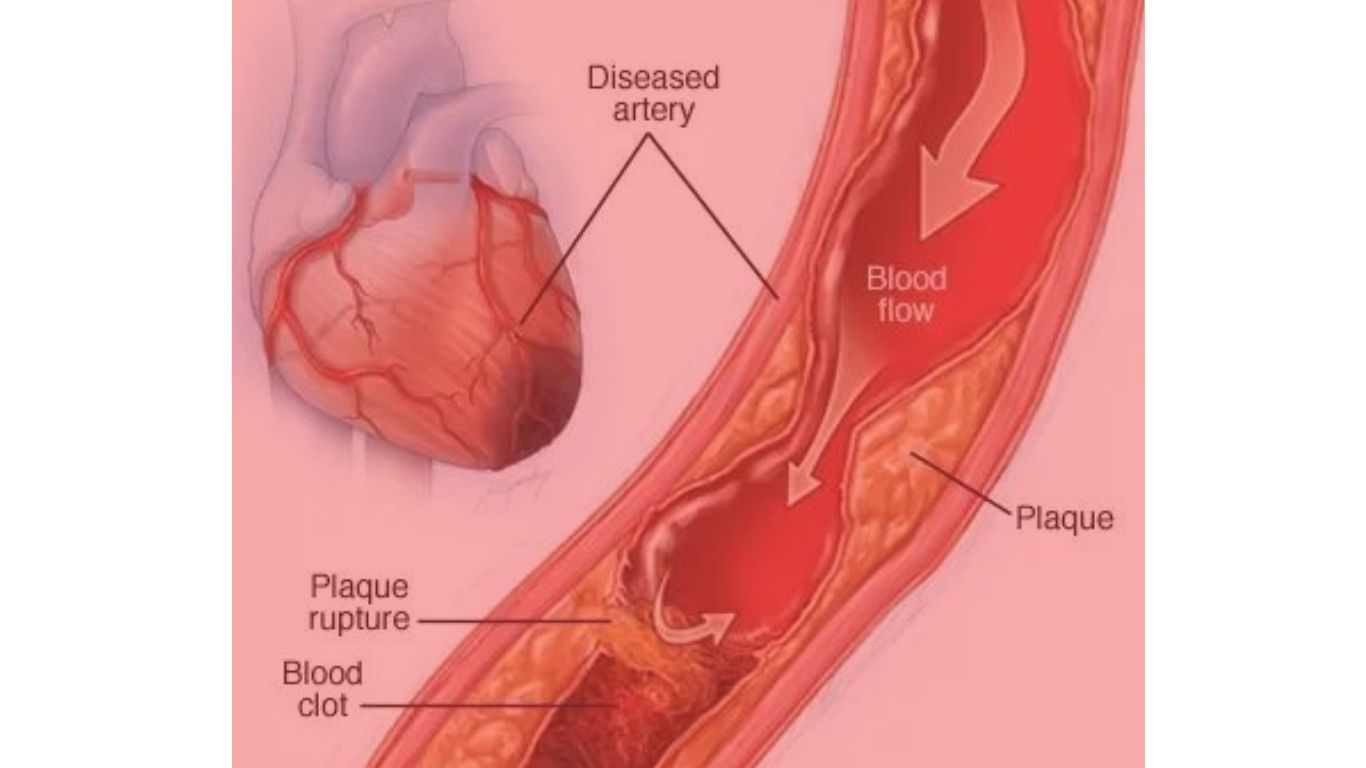
Coronary thrombosis refers to the formation of a blood clot (thrombus) within the coronary arteries. These arteries are responsible for supplying oxygenated blood to the heart muscle. When a clot forms, it obstructs the flow of blood, leading to ischemia (reduced blood flow) and potentially resulting in a myocardial infarction if the blockage is severe and prolonged.
1.2 What is Myocardial Infarction?
Myocardial infarction, or heart attack, occurs when blood flow to a part of the heart is completely blocked for an extended period, leading to the death of heart muscle tissue. This condition is a medical emergency and requires prompt treatment to restore blood flow and minimize damage to the heart.
2. Symptoms of Coronary Thrombosis and Myocardial Infarction
Recognizing the symptoms of coronary thrombosis and myocardial infarction is critical for seeking timely medical intervention. The symptoms can vary depending on the severity of the blockage and the area of the heart affected.
2.1 Common Symptoms
- Chest Pain or Discomfort: The most common symptom of myocardial infarction is chest pain or discomfort, often described as a feeling of pressure, squeezing, fullness, or pain in the center or left side of the chest. This pain may last for more than a few minutes or come and go.
- Pain in Other Parts of the Body: The pain or discomfort may radiate to other parts of the body, such as the arms (especially the left arm), back, neck, jaw, or stomach.
- Shortness of Breath: Difficulty breathing, or shortness of breath often accompanies chest pain. It can occur at rest or during physical activity.
- Sweating: Excessive sweating, particularly cold sweats, is a common symptom.
- Nausea and Vomiting: Some individuals may experience nausea, vomiting, or a feeling of indigestion.
- Lightheadedness or Dizziness: A feeling of lightheadedness, dizziness, or fainting can occur, especially in conjunction with other symptoms.
- Fatigue: Unusual or unexplained fatigue, particularly in women, can be an early sign of myocardial infarction.
2.2 Atypical Symptoms
While the symptoms mentioned above are common, some individuals, particularly women, the elderly, and people with diabetes, may experience atypical symptoms, such as:
- Atypical Chest Pain: The chest pain may be less severe or felt in unusual locations.
- Indigestion or Heartburn: Some people may mistake the pain for indigestion or heartburn.
- Palpitations: Irregular or rapid heartbeats may occur.
- Silent Myocardial Infarction: In some cases, myocardial infarction may occur without any noticeable symptoms, especially in individuals with diabetes.
3. Causes of Coronary Thrombosis and Myocardial Infarction
Understanding the causes of coronary thrombosis and myocardial infarction is essential for prevention and risk reduction.
3.1 Atherosclerosis
The primary cause of coronary thrombosis and myocardial infarction is atherosclerosis, a condition characterized by the buildup of fatty deposits (plaques) within the walls of the coronary arteries. Over time, these plaques harden and narrow the arteries, reducing blood flow to the heart. If a plaque ruptures, a blood clot can form at the site, leading to a complete blockage of the artery.
3.2 Risk Factors for Atherosclerosis
Several factors contribute to the development of atherosclerosis, including:
- High Blood Pressure (Hypertension): Elevated blood pressure damages the inner lining of the arteries, making them more susceptible to plaque buildup.
- High Cholesterol Levels: High levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol, contribute to plaque formation in the arteries.
- Smoking: Smoking damages the blood vessels and promotes the buildup of fatty deposits in the arteries.
- Diabetes: Diabetes increases the risk of atherosclerosis by promoting inflammation and damaging the blood vessels.
- Obesity: Excess body weight is associated with increased cholesterol levels, high blood pressure, and insulin resistance, all of which contribute to atherosclerosis.
- Sedentary Lifestyle: Lack of physical activity can lead to obesity and other risk factors for atherosclerosis.
- Unhealthy Diet: A diet high in saturated fats, trans fats, and processed foods contributes to elevated cholesterol levels and plaque formation.
- Family History: A family history of heart disease increases the risk of developing atherosclerosis and myocardial infarction.
- Age: The risk of atherosclerosis increases with age, as the arteries naturally become less flexible and more prone to plaque buildup.
- Gender: Men are at a higher risk of developing coronary artery disease at a younger age compared to women. However, the risk for women increases after menopause.
3.3 Other Contributing Factors
In addition to atherosclerosis, other factors can trigger coronary thrombosis and myocardial infarction, including:
- Vasospasm: A sudden spasm of a coronary artery can temporarily restrict blood flow to the heart, leading to ischemia and potentially triggering a heart attack.
- Coronary Artery Dissection: A tear in the inner layer of a coronary artery can cause blood to accumulate between the layers, leading to a blockage and myocardial infarction.
- Hypercoagulability: Certain conditions or medications can increase the tendency of the blood to clot, raising the risk of coronary thrombosis.
4. Effects of Coronary Thrombosis and Myocardial Infarction
The effects of coronary thrombosis and myocardial infarction can be profound, impacting not only the heart but also other organs and overall health.
4.1 Immediate Effects
- Heart Muscle Damage: The most immediate effect of myocardial infarction is damage to the heart muscle. The extent of the damage depends on the size of the affected area and the duration of the blockage. If a significant portion of the heart muscle is damaged, it can impair the heart’s ability to pump blood effectively.
- Arrhythmias: Myocardial infarction can lead to irregular heart rhythms, known as arrhythmias. Some arrhythmias are minor, but others, such as ventricular fibrillation, can be life-threatening and require immediate medical intervention.
- Cardiogenic Shock: In severe cases, myocardial infarction can lead to cardiogenic shock, a condition where the heart is unable to pump enough blood to meet the body’s needs. This can result in organ failure and is a medical emergency.
- Heart Failure: Myocardial infarction can weaken the heart muscle, leading to heart failure. In heart failure, the heart is unable to pump blood efficiently, causing fluid buildup in the lungs, legs, and other parts of the body.
- Pericarditis: Inflammation of the pericardium, the sac surrounding the heart, can occur after myocardial infarction, leading to chest pain and other symptoms.
4.2 Long-term Effects
- Reduced Quality of Life: Survivors of myocardial infarction may experience a reduced quality of life due to ongoing symptoms, such as fatigue, shortness of breath, and chest discomfort.
- Increased Risk of Future Heart Attacks: Individuals who have had one myocardial infarction are at a higher risk of experiencing another heart attack in the future.
- Emotional and Psychological Impact: Surviving a heart attack can have a significant emotional and psychological impact, leading to anxiety, depression, and fear of recurrence.
- Lifestyle Changes: To prevent future heart attacks, individuals may need to make significant lifestyle changes, such as adopting a heart-healthy diet, quitting smoking, and increasing physical activity.
5. Prevention of Coronary Thrombosis and Myocardial Infarction
Prevention of coronary thrombosis and myocardial infarction involves addressing the risk factors and making lifestyle changes to promote heart health.
5.1 Lifestyle Modifications
- Healthy Diet: Adopting a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help lower cholesterol levels, reduce blood pressure, and prevent atherosclerosis. The Mediterranean diet, which emphasizes olive oil, nuts, fish, and plant-based foods, is particularly beneficial for heart health.
- Regular Exercise: Engaging in regular physical activity, such as brisk walking, swimming, or cycling, helps maintain a healthy weight, lowers blood pressure, and improves cholesterol levels. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Weight Management: Maintaining a healthy weight reduces the risk of high blood pressure, diabetes, and high cholesterol, all of which contribute to atherosclerosis.
- Smoking Cessation: Quitting smoking is one of the most important steps in preventing coronary artery disease and myocardial infarction. Smoking cessation programs, medications, and support groups can help individuals quit successfully.
- Stress Management: Chronic stress can contribute to high blood pressure and unhealthy behaviors, such as overeating or smoking. Stress management techniques, such as mindfulness, meditation, yoga, and deep breathing exercises, can help reduce stress levels and improve heart health.
- Limit Alcohol Consumption: Excessive alcohol consumption can raise blood pressure and contribute to heart disease. Limit alcohol intake to moderate levels, defined as up to one drink per day for women and up to two drinks per day for men.
5.2 Medical Interventions
- Medications: Individuals at high risk of coronary thrombosis and myocardial infarction may be prescribed medications to manage risk factors, such as high blood pressure, high cholesterol, and diabetes. Common medications include statins, beta-blockers, ACE inhibitors, and aspirin.
- Regular Health Screenings: Regular check-ups with a healthcare provider can help monitor blood pressure, cholesterol levels, and blood sugar levels, allowing for early detection and management of risk factors.
- Managing Chronic Conditions: Effectively managing chronic conditions, such as diabetes, hypertension, and high cholesterol, is crucial for preventing coronary artery disease and myocardial infarction.
6. Homeopathic Remedies for Coronary Thrombosis and Myocardial Infarction
Homeopathy is a holistic approach to medicine that aims to stimulate the body’s natural healing processes. Homeopathic remedies are selected based on the individual’s symptoms, constitution, and overall health. While homeopathy can be used as a complementary approach to conventional medicine, it is important to note that it should not replace emergency medical treatment for myocardial infarction.
6.1 Commonly Used Homeopathic Remedies
- Arnica montana: Arnica is often used for trauma, shock, and injury. It may be indicated in the early stages of myocardial infarction, particularly if there is a feeling of soreness or bruising in the chest.
- Aconitum napellus: Aconite is used for sudden onset conditions with intense fear and anxiety. It may be helpful in the acute phase of myocardial infarction, especially if the individual experiences extreme fear of death, palpitations, and restlessness.
- Cactus grandiflorus: This remedy is indicated for conditions affecting the heart and blood vessels. It may be used for angina, myocardial infarction, and other heart conditions characterized by a constricting or squeezing sensation in the chest, as if the heart is being compressed.
- Lachesis mutus: Lachesis is used for circulatory and cardiac conditions, especially when there is a tendency toward clot formation. It may be indicated in cases of myocardial infarction where there is a sense of constriction, tightness, or oppression in the chest, along with difficulty breathing.
- Crataegus oxyacantha: Commonly known as hawthorn, this remedy is often used to support heart health. It may be helpful in cases of myocardial infarction, particularly in the recovery phase, as it is believed to strengthen the heart muscle and improve circulation.
- Digitalis purpurea: Digitalis is used for heart conditions characterized by a weak, irregular, or slow pulse. It may be indicated in cases of myocardial infarction with symptoms of heart failure, such as shortness of breath, palpitations, and edema.
- Spigelia anthelmia: This remedy is indicated for sharp, stabbing chest pain that radiates to the left arm or shoulder, resembling the symptoms of myocardial infarction. It may be used for angina and other heart conditions.
6.2 Homeopathic Case-Taking and Individualization
Homeopathy is highly individualized, meaning that the selection of a remedy is based on the unique symptoms and constitution of the individual. A homeopath will take a detailed case history, including physical, emotional, and mental symptoms, before prescribing a remedy. In acute cases, such as myocardial infarction, the focus is on matching the most characteristic symptoms with the appropriate remedy.
6.3 Complementary Role of Homeopathy
While homeopathy may offer supportive care during the recovery phase of myocardial infarction, it is crucial to understand that it should not be used as a substitute for emergency medical care. If someone is experiencing symptoms of a heart attack, it is imperative to seek immediate medical attention by calling emergency services.
7.FAQs about Homeopathic Remedies for Coronary Thrombosis
Q1: What is coronary thrombosis, and how can homeopathic remedies help?
A1: Coronary thrombosis is the formation of a blood clot in one of the coronary arteries, which can obstruct blood flow to the heart muscle, leading to a heart attack. Homeopathic remedies aim to support the body’s natural healing processes, potentially improving circulation, reducing inflammation, and preventing further clot formation. However, homeopathy should be used as a complementary approach alongside conventional medical treatments for coronary thrombosis.
Q2: Can homeopathic remedies prevent coronary thrombosis?
A2: Homeopathic remedies may help address underlying factors that contribute to the development of coronary thrombosis, such as high cholesterol, hypertension, and stress. Remedies like Crataegus or Arnica Montana are often recommended for heart health. However, prevention of coronary thrombosis primarily relies on lifestyle changes, such as a healthy diet, regular exercise, and adherence to prescribed medications.
Q3: Which homeopathic remedies are commonly used for coronary thrombosis?
A3: Some common homeopathic remedies used for conditions related to coronary thrombosis include Arnica Montana for reducing inflammation, Aconitum Napellus for sudden onset of symptoms like chest pain, and Crataegus for strengthening the heart muscle and improving circulation. Lachesis Mutus is also used for its blood-thinning properties.
Q4: Are there any side effects associated with homeopathic remedies for coronary thrombosis?
A4: Homeopathic remedies are highly diluted, making side effects rare. However, individuals may experience an initial aggravation of symptoms before improvement occurs. It is essential to use these remedies under the guidance of a qualified homeopath, especially when dealing with serious conditions like coronary thrombosis.
Q5: Can homeopathic remedies be used alongside conventional medications for coronary thrombosis?
A5: Yes, homeopathic remedies can be used as a complementary therapy alongside conventional medications. However, it is crucial to consult both your homeopath and your healthcare provider to ensure there are no interactions or contraindications between the homeopathic remedies and prescribed medications.
Q6: How long does it take to see results from homeopathic treatment for coronary thrombosis?
A6: The timeframe for seeing results from homeopathic treatment varies depending on the individual, the severity of the condition, and the remedy used. Some individuals may notice improvement within a few weeks, while others may require longer treatment periods. Continuous monitoring and follow-up with a homeopath are essential for adjusting the treatment plan as needed.
Q7: Is it safe to self-prescribe homeopathic remedies for coronary thrombosis?
A7: Self-prescribing homeopathic remedies for a serious condition like coronary thrombosis is not recommended. It is important to seek the advice of a qualified homeopath who can assess your symptoms, consider your medical history, and recommend appropriate remedies. Self-prescribing without proper guidance may result in ineffective treatment or worsening of symptoms.
Q8: Are there specific lifestyle changes recommended alongside homeopathic treatment for coronary thrombosis?
A8: Yes, lifestyle changes are crucial for managing coronary thrombosis. These include adopting a heart-healthy diet rich in fruits, vegetables, and whole grains; regular physical activity; stress management techniques such as meditation or yoga; quitting smoking; and limiting alcohol intake. Homeopathic treatment can be more effective when combined with these positive lifestyle changes.
Q9: Can homeopathy cure coronary thrombosis completely?
A9: Homeopathy aims to support the body’s natural healing processes and may alleviate symptoms or improve overall heart health, but it is not a standalone cure for coronary thrombosis. This condition requires comprehensive medical care, including conventional treatments like medications, lifestyle changes, and possibly surgical interventions. Homeopathy can be part of a holistic approach but should not replace conventional medical care.
Q10: What should I do if I suspect I have coronary thrombosis and want to use homeopathy?
A10: If you suspect you have coronary thrombosis, seek immediate medical attention as it is a potentially life-threatening condition. Once stabilized, you can consult with a qualified homeopath to discuss complementary homeopathic treatments that may support your recovery and overall heart health. It is important to prioritize emergency care and follow the advice of your healthcare providers.
Conclusion
Coronary thrombosis and myocardial infarction are serious medical conditions that require prompt recognition, treatment, and prevention. Understanding the symptoms, causes, and effects of these conditions can help individuals take proactive steps to reduce their risk and improve their heart health. While homeopathy may offer complementary support, particularly in the recovery phase, it should be used in conjunction with conventional medical care.
Preventive measures, such as adopting a heart-healthy lifestyle, managing chronic conditions, and seeking regular medical check-ups, are essential for reducing the risk of coronary artery disease and myocardial infarction. By taking these steps, individuals can protect their heart health and reduce the likelihood of experiencing a heart attack, ultimately leading to a longer, healthier life.